Inheritance
APECED is inherited in an autosomal recessive manner. In autosomal recessive inheritance, an affected person has a variant in each of their two copies of the AIRE gene—one inherited from the mother and one from the father. Typically, both parents of an affected person carry one abnormal AIRE gene and are unaffected by the disease. When both parents are carriers, each child has a 25%, or one in four, chance of being affected by the disease. Sometimes the two copies of the AIRE gene that a child inherits have identical, or homozygous, variants. Most North American individuals with APECED have different variants on the two copies of AIRE, called compound heterozygous variants. In either case, they are not able to produce functional AIRE protein.
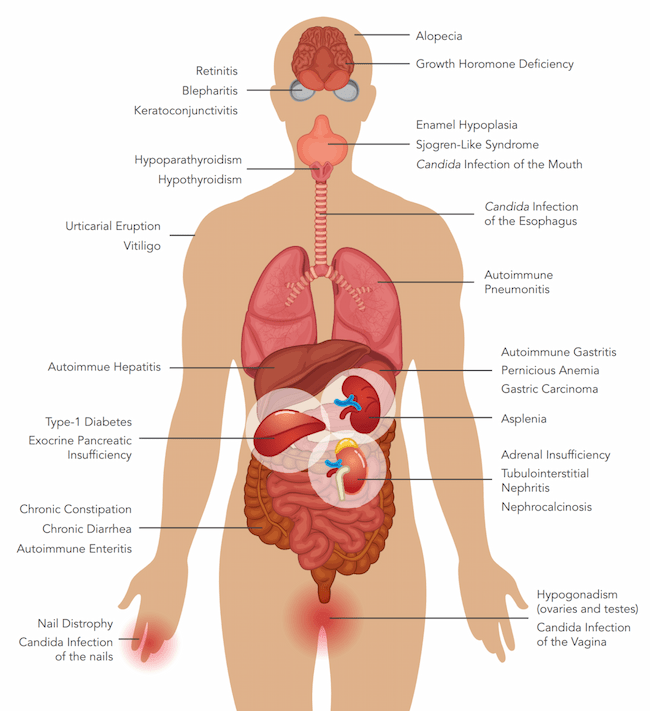
Recent evidence suggests that in some individuals who present with APECED-like clinical manifestations, the disease is inherited in an autosomal dominant manner. In autosomal dominant inheritance, an affected person has a variant in one of their two copies of the AIRE gene. The variant is inherited from a parent who is also affected by the syndrome. The other parent does not carry a variant in the AIRE gene and is healthy. In this situation, each child has a 50% chance of being affected by the disease. Such mutations have been reported in European individuals, but so far have not been observed in North American individuals with APECED. The individuals do not typically present with the full-blown APECED syndrome but instead develop organ-specific autoimmune manifestations that are seen in APECED, such as vitiligo, B12 deficiency, or an endocrine disorder.
About 15% of North American individuals with a clinical APECED diagnosis do not have detectable variants or deletions in both copies of the coding regions of the AIRE gene, suggesting that other undiscovered genetic factors may be involved in the syndrome. Further research is needed to understand the genetic factors (non-coding AIRE elements or non-AIRE genes) that contribute to APECED in families without biallelic AIRE gene variants; a biallelic variant is a variant but not necessarily the same variant in both copies of a particular gene (a paternal and a maternal variant).