
-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can live with the disease or support others in your life with PI. Learn more about PI, including the various diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Research Grant Program
-
Consulting immunologist
-
Diagnosing PI
-
Getting prior authorization
-
Clinician education
-
Survey research
-
Participating in clinical trials

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Research Grant Program
Dr. Elizabeth Younger sees hundreds of patients who require immunoglobulin (Ig) replacement therapy and no two use the same brand, amount, and type of administration. Ig replacement therapy provides antibodies, specifically immunoglobulin G (IgG), to persons who have low IgG, including those with primary immunodeficiencies.
“I have 500 patients on immunoglobulin replacement therapy, and I laughingly say I probably have 500 different infusion regimens because everybody’s taken the infusion regimen and tweaked it and made it their own and if any of my patients are out there in that audience, they will all shake their heads yes,” said Younger, assistant professor of pediatrics, Johns Hopkins School of Medicine, and member of the IDF Nurse Advisory Committee, during a recent IDF Forum “Immunoglobulin (Ig) Replacement Therapy: As Individual as You.”
“After I teach them the procedure for infusion, I say that’s the least important thing that I’m teaching you. The most important thing that I teach you in this session is to take control of this, make it your own, decide what it looks like for you, and I will help you make it look that way and that’s the conversation that needs to happen.”
Ig replacement therapy is manufactured from plasma collected from donors, which contains antibodies against diseases the donors have had or against which they’ve been vaccinated. While each lot number of each brand is a little bit different, in general, the solution of antibodies protects against diseases like the common cold, measles, tetanus, and, most recently, COVID-19, said Young.
“Since November, there’s been COVID antibody and the COVID antibody rises with every lot number that comes off the conveyor belt,” said Younger.
Ig replacement therapy contains between 95 and 99 percent IgG, and very little IgA or IgM. The therapy is designed to provide a person with antibodies lacking in their own body, and it won’t help them produce their own antibodies, nor will it clear up acute infections.
“When I start new patients on therapy, they always say, ‘Well how long will it take before my own system kicks back in?’ It isn’t going to kick back in or cure any antibody deficiency; it just gives you what you can’t make for yourself or supplements what you already have,” said Younger.
Ig replacement therapy is given through needles into the body in one of three ways:
Intravenous immunoglobulin (IVIg) is administered into the bloodstream through a vein every three to four weeks.
Subcutaneous immunoglobulin (SCIg) is administered under the skin every one to 14 days.
Facilitated subcutaneous immunoglobulin (SCIg FAC) is administered under the skin every two to four weeks. SCIg FAC allows a person to administer a larger volume of Ig by injecting a material that increases absorption.
Choosing how it is administered and the timing are only two of many choices a person must make when it comes to Ig replacement therapy. Other considerations include:
Do you want to administer the IgG yourself at home (SCIg or SCIg FAC only), have a provider visit the home to assist with administration, or visit a hospital-based or free-standing infusion site where providers will administer the product?
Which product should you use? There are multiple products on the market. All are FDA-approved, safe, and created from plasma collected in the United States.
How long does the administration take?
What are the side effects?
What is the cost difference and what does insurance cover?
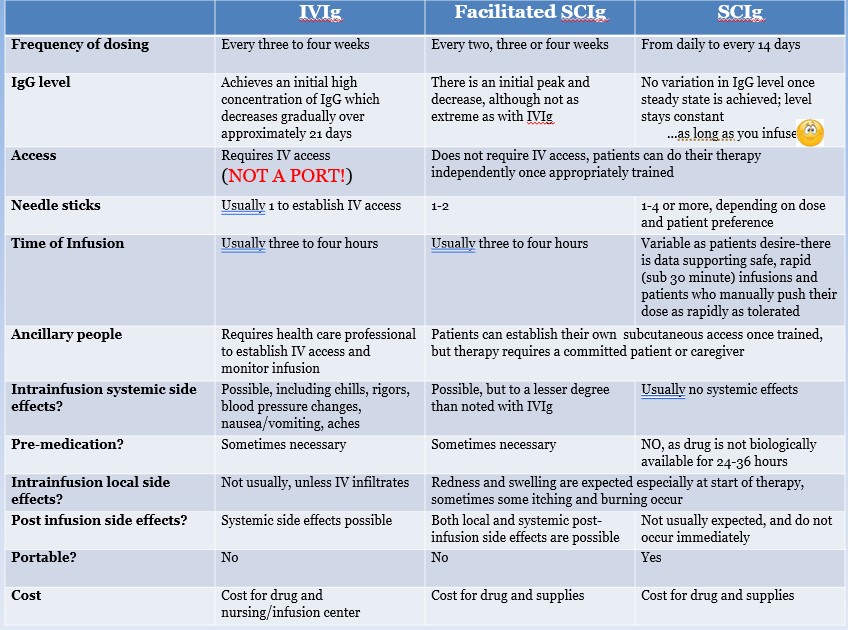
“Thinking about the differences and options, whether they’re clinically important or advantages or disadvantages should be determined by the prescriber and the patient,” said Younger. “I never call things advantages or disadvantages. I talk about differences, and what’s an advantage for me might be a disadvantage for you.”
There are many ways to give a dose of Ig replacement therapy based on type, how much, how often, and when, said Younger, and if you’re unhappy with your regimen, then meet with your prescriber and determine how you can tailor it.
“If you hate your infusion regimen, part of that is on you. You need to be your own advocate. Have a discussion with your prescriber and say, ‘Listen, I really hate this. I dread it every week. I don’t want to do it.’ And the question needs to be asked, ‘What can we do to make it better?’ If you don’t have that discussion, then nobody can fix your problem,” said Younger.
The goal of Ig replacement therapy is to protect against severe and/or frequent infections, like pneumonia, and while you may get the occasional cold or sinus infection, therapy should allow you the freedom to participate in activities that make you happy and that you find fulfilling.
“Most importantly, it’s to give you therapy that will help you live the life you want to live. So many people come to us who have been sick for so many years and they’re just sick and tired of being sick and tired all the time, and we put them on therapy, and we really hope to change their lives and give them the life they want to lead back again,” said Younger.
Topics
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.





The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309



