
-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can live with the disease or support others in your life with PI. Learn more about PI, including the various diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Research Grant Program
-
Consulting immunologist
-
Diagnosing PI
-
Getting prior authorization
-
Clinician education
-
Survey research
-
Participating in clinical trials

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Research Grant Program
What happens when drugs that help treat infectious diseases stop working? While a return to the pre-antibiotic era of medicine would be unfortunate for the general public, it could be catastrophic for those with compromised immune systems.
Antibiotics, which target bacteria, were the first type of medicine developed to treat infectious diseases. Collectively, drugs that treat infectious diseases are known as antimicrobials, and also include antivirals to treat viruses (e.g., AIDS), antifungal medications for fungi (e.g., athlete’s foot), and antiparasitics for parasites (e.g., pinworm).
Many antimicrobials are actually natural compounds that microorganisms have used against each other for millions of years in their fight for limited resources. For example, Penicillium molds make penicillin to kill off bacterial competitors; Alexander Flemming just happened to see this in action when mold took over one of his experiments.
But now, antimicrobials are increasingly failing to treat infections. For the past three years, antimicrobial resistance, or the ability of microorganisms to survive antimicrobial treatment, consistently made the World Health Organization (WHO)’s list of top 10 global health threats. The U.S. Centers for Disease Control and Prevention (CDC) estimates that 2.8 million antibiotic-resistant infections occur in the U.S. each year, resulting in 35,000 deaths.
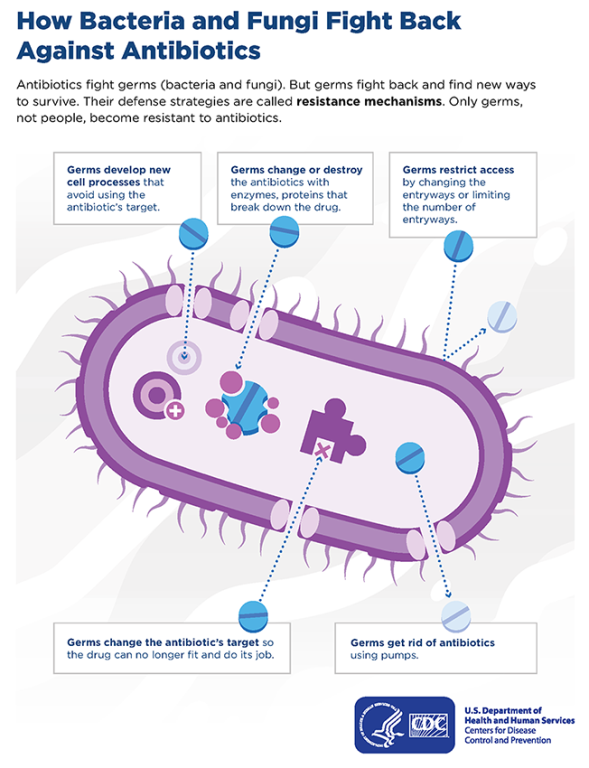
When someone has an infection that is resistant to antimicrobials, it is the microorganisms themselves that ‘resist’ the drug, not the patient’s body. Typically, resistant microorganisms have either acquired a new gene that helps neutralize the antimicrobial or adapted their own set of genes over many, many generations. The problem is that the time between microbial generations can be as short as 20 minutes.
It’s not surprising then that scientists often identify microorganisms with resistance to a given antimicrobial within a few years of widespread use of the drug. Some microorganisms, like certain strains of the bacteria that cause tuberculosis, have even become resistant to multiple drugs. The nightmare scenario (and focus of many ‘superbug’ media stories) is the spread of a microorganism that is resistant to all antimicrobials currently available to treat it.
People with primary immunodeficiencies, as well as others who are immunocompromised, are particularly at risk of acquiring antimicrobial-resistant infections. Many rely on the prophylactic use of antimicrobials to prevent infection. Not only may these drugs become less effective as preventative measures, but there is already evidence that resulting infections are harder to treat.
The WHO and the U.S. CDC have action plans in place to curb the spread of antimicrobial resistance at the national and international levels, but individual actions can help too. Take antimicrobials only as they are prescribed to you, and take other steps to prevent infection, like washing your hands well and keeping your pets healthy.
Topics
Related resources

Foundation provides guidance amid changing vaccine recommendations

Education policy changes could impact students with PI

Foundation to follow medical societies' vaccine schedules in light of ACIP hepatitis B decision
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.





The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309

