-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can live with the disease or support others in your life with PI. Learn more about PI, including the various diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Research Grant Program
-
Consulting immunologist
-
Diagnosing PI
-
Getting prior authorization
-
Clinician education
-
Survey research
-
Participating in clinical trials

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Research Grant Program
Some children with severe combined immunodeficiency (SCID) who are treated with bone marrow transplant (BMT) require immunoglobulin infusions for months, sometimes years, after the transplant. But why? And what can parents expect as their child recovers from the transplant and builds a new immune system from donor cells?

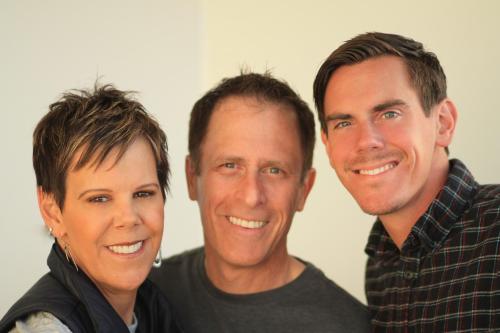
Two SCID experts, Dr. Manish Butte, Division Chief of Immunology, Allergy, and Rheumatology at the University of California Los Angeles, along with Dr. Victoria Dimitriades, Division Chief of Pediatric Allergy, Immunology, and Rheumatology at the University of California Davis Children’s Hospital, explored answers to these questions in “B Cell Reconstitution and IgG Replacement Therapy,” a presentation offered by IDF’s SCID Compass program.
Butte said that to understand how B cell reconstitution works, it’s important to examine the immune system and SCID itself.
All babies with SCID have no T cells, but depending on the type of SCID, a child may be missing only T cells or missing both T cells and B cells. Even when a child does have B cells, usually those B cells don’t work well, and that’s because T and B cells have to work together to make antibodies and fight infection properly.
“That’s why we call this a severe combined immune deficiency because the T cell arm of the immune response and the B cell arm of the immune response are both broken when the T cells are missing,” explained Butte.
A BMT provides a baby with SCID donated stem cells to replace their own stem cells that carry the affected gene. The goal is for the donated stem cells to make healthy T cells and B cells, which develop into a replacement immune system for the baby.
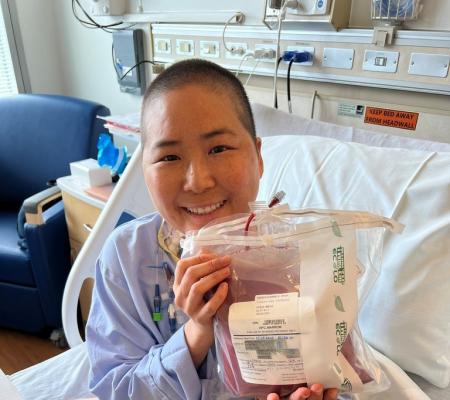
Day 0 is when a baby receives the infusion of the new stem cells into their vein during the transplant. Those stem cells find their way into the baby’s bone marrow and begin to form new blood cells, a process called engraftment.
Not all the new blood cells are made at the same time, and the baby needs to be hospitalized for weeks, and sometimes months, after the transplant as doctors wait for the blood cells to come online and start growing from the new stem cells, explained Butte.
The first blood cells that start to form are the neutrophils, usually within the first two weeks, and red blood cells, platelets, and other cells start appearing within the first month. T cells start to show up in good numbers at about three months, around Day 100 after the transplant, said Butte, and B cells take even longer to come online.
“There are many patients that don’t start making B cells even in small numbers in about three or four months. And in many of our patients, it can be six months or more before they’re really starting to crank out an appreciable number of B cells,” said Butte.
“In fact, even though we have discharged many of these babies home from the hospital, they may be spending the next few months or years continuing to grow enough B cells in their blood that they can then fight infections and be able to handle vaccines.” Even when a baby starts producing B cells, sometimes those B cells aren’t fully functional, which means they haven’t matured into memory B cells and plasma cells.
“It really can in many cases take patients two years before you start making enough plasma cells and memory B cells that the vaccines will actually take,” said Butte.
That’s why some babies with SCID treated with BMT need to receive Ig replacement therapy for months or years after transplant. The Ig provides them with the antibodies they need to fight infection because they are not making functional B cells yet.
“Typically, B cells make antibodies on their surface, and then they float around the blood looking for infections. When they sense an infection, they can secrete those antibodies, and the levels of antibodies can go up in the blood during infections because these B cells are cranking out antibodies,” said Butte.
“The key is, can they outgrow the need for immunoglobulin? Can you make enough B cells after the transplant, and can those B cells be functional enough that the need to have other people’s Ig being provided can fade away? And this is really still an open question we’re trying to solve in the treatment of babies with SCID.”
According to studies, the following are factors that influence B cell reconstitution after SCID BMT:
Conditioning agent
The major factor affecting B cell function after transplant is the type of SCID.
“There are some genetic causes of SCID that really break B cells badly and thus it requires a whole fresh new immune system including a good number of B cells to grow anew before you even have a chance of making good B cell function, antibody production, and vaccine responses,” said Butte.
The second most important factor influencing B cell function is whether or not chemotherapy, also known as conditioning, is used before the transplant. Conditioning makes space in the bone marrow of the baby and promotes engraftment.
The third factor affecting B cell function is the chemotherapy agent used in the conditioning.
“We’ve really focused in the field on this one chemotherapy agent called busulfan, a very powerful chemotherapy and it seems to be one of the most important for getting rid of the bone marrow in a way that allows new bone marrow to grow and especially new B cells to grow,” said Butte.
“There is now an ongoing trial that allows our field all over the world to learn by giving children with SCID different doses of busulfan or not and tracking their B cell development afterward based on genetics, and based on other factors to try to understand what’s the best dose of busulfan - a low dose, a medium dose, to try to get the B cells to grow and yet producing the least amount of harm.”
After a BMT, if a child isn’t producing functional B cells, then they can receive Ig replacement therapy, which is donated plasma that undergoes a filtration process and is used to provide antibodies to those who lack them. Ig therapy is administrated either subcutaneously or intravenously, and both have their pros and cons.
Intravenous immunoglobulin (IVIg) is administered in the vein every three to four weeks, usually in a medical facility. If the child has an existing catheter, that can be used. Otherwise, IV placement is required each month. Infusions can take three to four hours. When given in this way, Ig slowly goes up in the body, peaks, and then drops down, with lower protection the week before the next infusion.
Subcutaneous Immunoglobulin (SCIg) is administered under the skin every one to two weeks in areas including the thighs, abdomen, and arms. Infusions take 30 minutes to two hours and can be done at home by a caretaker. The SCIg circulates in the body at a more consistent level than IVIg.
“When you give SCIg, you have fewer ups and down as compared to IVIg. It’s more in this nice consistency of IgG level instead of the spiking of the IVIg. We tend to like that. Although the highs are nice when you get IVIg, the lows can put you in a more precarious place in terms of your infection risk. So, sometimes we prefer to use SCIg to keep a more moderate level,” said Dimitriades.
There is a standard dose for Ig but expect that to vary based on the child.
“I want people to understand that this is an art and not a science when it comes to dosing. We aim for a general amount, usually around 500 milligrams for every kilogram of weight but after dosing, we look at the patient’s daily experience, infection risks, and things like that to adjust the dose to make sure we’re giving them the optimal amount that they need. Every patient is a little bit different,” said Dimitriades.
Finally, children who need Ig therapy long-term will have follow-up appointments every six to 12 months where doctors check blood counts, blood chemistry, and IgG levels, review any infections, discuss side effects, and determine if vaccines are appropriate.
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.





The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309