-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can live with the disease or support others in your life with PI. Learn more about PI, including the various diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Research Grant Program
-
Consulting immunologist
-
Diagnosing PI
-
Getting prior authorization
-
Clinician education
-
Survey research
-
Participating in clinical trials

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Research Grant Program
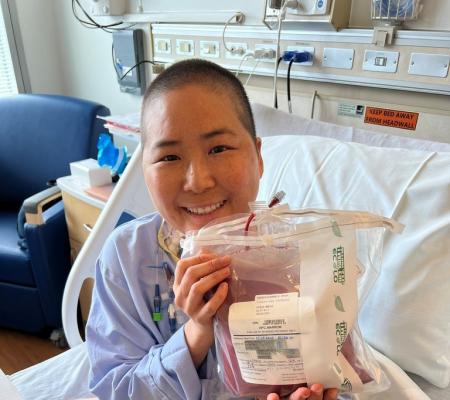
Just because a person with severe combined immunodeficiency (SCID) receives a bone marrow transplant (BMT), or gene therapy, for their condition, that doesn’t mark an end to their journey with SCID. As the years and decades pass, it’s imperative that they monitor their health to ensure that not only is their immune system working properly, but also that they identify any side effects that could arise from the SCID diagnosis and treatment.
Dr. Jennifer Heimall explored the reasons why people with SCID should keep a close watch on their health through the years, during her discussion “Post-Transplant Late Effects in Patients with SCID” at the IDF Rare of the Rare conference in October 2021. Dr. Heimall is an attending physician in the Division of Allergy and Immunology at the Children’s Hospital of Philadelphia and an assistant professor of clinical pediatrics at the University of Pennsylvania’s Perelman School of Medicine.
SCID is characterized by a lack of T cells, resulting in little to no functioning immune system. The only treatment is to provide an immune system through donor stem cells in a BMT, or through the patient’s own corrected stem cells in gene therapy, which is still in clinical trials. SCID is fatal for babies unless they are treated with BMT or gene therapy.
While the first bone marrow transplants for SCID took place in 1968, few studies have followed patients long-term to determine the status of their health. Most follow-up with bone marrow transplant is focused on people who received BMT for cancer.
Nonetheless, the post-transplant late effects of SCID do overlap with those related to cancer, according to studies. Those include:
- Neuro-psychological late effects such as learning delays
- Lung disease and kidney disease
- Bone and growth abnormalities
- Development of endocrine issues
- Concern for infectious disease
- Concerns of gonadal dysfunction and infertility due to conditioning
- Liver disease
- Cardiovascular disease
- Solid cancers
A primary difference in transplanting a person with SCID versus a person with cancer is that those with SCID receive their transplants in infancy, ideally within the first few months of life.
“When we talk with families in the pre-transplant time period about what are the risks, the thing we need to focus on is that this is a transplant being performed during infancy and that is still a relatively rare thing to have happen,” said Dr. Hiemall.
How will graft versus host disease affect the baby? What are the effects of conditioning at such a young age? What comorbidities (such as a heart condition or kidney disease) exist in the baby?
“When we follow these patients over time we need to consider the durability of the immune reconstitution achieved and how that might be different based on the type of graft used and the type of conditioning,” said Dr. Heimall.
How the SCID genotype impacts other organs must also be considered when examining the late effects of SCID.
“It’s very important that families and patients, as they become older, are counseled that there is still an ability to pass on the genetic variants that caused SCID for the patients to future generations because we haven’t replaced every cell in the body. We only replaced the immune system with a transplant,” explained Dr. Heimall.
Guidelines and recommendations for long-term screening and management of SCID patients treated with BMT stress the reassessment of the immune system.
“We know that the person (with SCID) is followed closely by the transplant team and potentially immunology team as well, but only to a certain point and every center is slightly different. Some may follow three years post-transplant, some follow for five years, but at some point, most centers will graduate their patients from being followed by the transplant team to then being followed by an oncology survivorship group to look for late effects that are known to be associated with exposure to chemotherapy and that are known to be associated with a BMT,” explained Dr. Heimall.
“But those groups may not be thinking through the lens of immunology and thinking through the lens of transplant for this non-malignant primary immunodeficiency indication. So, we wanted to really emphasize that it’s important for these elements of the immune reconstitution to be evaluated through serology over time, certainly starting no later than three months after transplant but then continued lifelong to make sure we’re constantly checking on the health of the graft.”
Assessing both T and B cell immune reconstitution is very important, and can be performed through most commercially available labs, said Dr. Heimall. She stressed that the tests should not measure just the overall engraftment, but lineage-specific engraftment, which measures T cell engraftment, B cell engraftment, and myeloid chimerism, which shows the level of donor-produced T and B cells and recipient-produced T and B cells.
“If you do overall engraftment, you won’t be able to see all the lineage-specific changes,” said Heimall.
Other aspects of health that persons with SCID should be particularly aware of as they follow their health long term are:
- Assessment for growth – The height and weight of persons with SCID should be monitored at least annually, and more frequently for those requiring nutritional support or showing evidence of slow growth or falling percentiles on the growth curve.
- Neuropsychologic development – Pediatricians should ensure that children are following age-appropriate guidelines for normal development and act early to refer for supportive therapies such as occupational therapy, physical therapy, or cognitive play therapy. Children should also have at least one formal neurocognitive assessment at about age 5 to determine if supportive therapies are needed. Testing can be done at the transplant center or through a school system.
- Lung diseases – These are more common if a person with SCID has had difficulty with infection, particularly lung infection prior to the transplant or if they are on long-term intravenous immune globulin (IVIG). Persons with SCID who have a need for long-term IVIG are at greater risk of having recurrent ear infections, sinus infections, and lung infections that can, over time, lead to more risk of lung disease.
- Thyroid disease – This is more common with exposure to certain conditioning agents and can lead to difficulty with gonadal dysfunction or infertility. It’s important to have an endocrine assessment when a child with SCID reaches puberty to make sure they’re going through normal development.
- Genetic testing – The SCID genotype should be established before transplant, but other options include keeping DNA for later testing or taking a skin biopsy after transplant for testing. Families should have genetic counseling to help them understand the reoccurrence of SCID within the family, and when a child with SCID is old enough, that child should also speak with a genetic counselor.
“The importance in the perception by the family and patients in what their health is and how the transplant has been effective for them or not is something we need to study and understand and make sure we are setting realistic expectations for families,” said Dr. Heimall.
Listen to “Post-Transplant Late Effects in Patients with SCID.”
Related resources
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.





The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309