
-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can live with the disease or support others in your life with PI. Learn more about PI, including the various diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Research Grant Program
-
Consulting immunologist
-
Diagnosing PI
-
Getting prior authorization
-
Clinician education
-
Survey research
-
Participating in clinical trials

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Research Grant Program
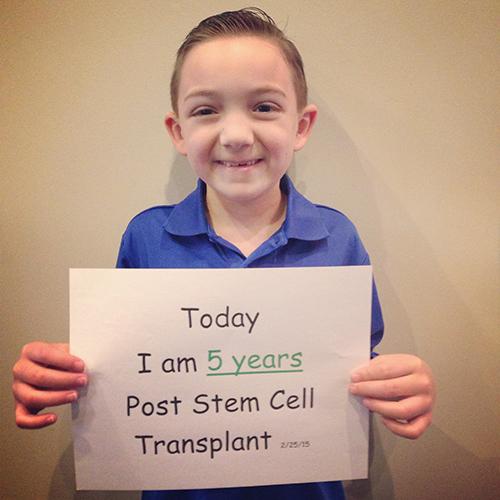
Today, Rocco Fernandez of River Ridge, Louisiana, is a happy and healthy six-year-old boy, who loves going to kindergarten and playing basketball with his dad. When looking at his beaming smile, it’s hard to believe that five years ago his life was very different.
Like many patients with chronic granulomatous disease (CGD), Rocco began to have mysterious health infections soon after he was born. At just three months old, he had a swollen lymph node in his neck, which was diagnosed as a staph infection. Doctors called it a “fluke” and prescribed antibiotics to treat it. However, his health did not improve.
Soon, his spleen and liver became enlarged. Then, at five months, Rocco developed a liver abscess. At this point, his doctors suspected that he had a severe immune deficiency, and after additional testing, Rocco was diagnosed with X-linked CGD.
Once they had processed the difficult news, Rocco’s parents, Melissa Layman-Fernandez and Chris Fernandez, began researching transplant options. From the outset, the family had more challenges to overcome. Rocco’s sister Laila was tested; she was not a match. Further, Rocco’s mixed Hispanic and Caucasian ethnicity meant fewer chances of finding a suitable unrelated donor in the bone marrow registries.
“Not one bone marrow match came up for Rocco,” said Melissa. “We knew at that point that an umbilical cord blood transplant was our only option.”
At the time, umbilical cord blood transplantation was a relatively new way to treat non-malignant diseases like CGD, and Melissa was not sure where to begin. She spoke to other mothers of children with CGD who had had transplants, and she credits organizations like IDF for helping parents of children with CGD connect and support one another.
“If it weren’t for the parents of children with CGD that I spoke to, I wouldn’t know what to do,” said Melissa. “We are a whole different community. It’s difficult to speak to someone who doesn’t know about CGD. They just look at you like a deer in the headlights.”
Melissa and her husband also researched top stem cell transplant centers across the country. They worked with Vinod Prasad, MD, MBBS, of the Pediatric Blood and Marrow Transplant Program at Duke University Medical Center.
Thanks to advancements in the field, today it is more common for patients like Rocco, who lack a suitable bone marrow donor, to undergo an umbilical cord blood transplant. In fact, recent data would suggest that the outcome of umbilical cord blood transplantation is comparable to that of matched unrelated donor transplantation with respect to the treatment of non-malignant diseases like CGD.
A cord blood match was found, and Rocco began a conditioning regimen under Dr. Prasad’s care in February of 2010. The transplant took place on the scheduled day, about two weeks later. Thankfully, Rocco responded well. His new cells engrafted, and he was discharged 28 days after the transplant. While Melissa was happy to take Rocco back to the apartment they had rented across the street from the hospital, she knew they were not out of the woods yet. The risk for complications from a transplant is highest during the first 100 days after transplant, when patients’ immune systems are unable to fight off infection.
Post-transplant, Melissa said Rocco had good days and bad days, as he began the process of recovering. She described it as “heartbreaking” at times, especially when Rocco lost interest in eating and began losing weight. Meanwhile, their transplant team kept a close watch on Rocco’s progress and adjusted his treatment as needed. Soon, Rocco’s health began to improve.
Finally, at 100 days post-transplant, the big day came. Lab reports showed that Rocco’s new immune system was working, and his transplant team delivered the news that Melissa had been waiting so long to hear: Rocco had a full oxidative burst. He was cured!
“My husband and I also had our anniversary on that day, and we were filled with so much emotion,” said Melissa. “We had no idea when we got married that we’d have this long, hard journey. But look how great Rocco is doing now. Everyone’s journey is different... I just want to give hope.”
Thank you to the Fernandez family for sharing their story! Hearing stories like this and meeting others living with CGD is so important.
Related resources

Man with X-linked hyper IgM first-ever to receive novel gene therapy

Pharmacist with CVID receives bone marrow transplant

Undiagnosed: Reuben & Sherri Johnson on CGD, chronic illness, and the fight for healthcare
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.





The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309

