-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can manage it. Learn about PI diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Research Grant Program
-
Consulting immunologist
-
Diagnosing PI
-
Getting prior authorization
-
Clinician education
-
Survey research
-
Participating in clinical trials

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Research Grant Program
When federal health officials added severe combined immunodeficiency (SCID) to the Recommended Uniform Screening Panel (RUSP), a national guideline for newborn screening (NBS), in 2010, it remained unclear to what degree NBS would improve outcomes for babies diagnosed with SCID.
Thirteen years later, a paper by the Primary Immune Deficiency Treatment Consortium (PIDTC) reveals that SCID identified through NBS increases overall survival for babies born with the condition.
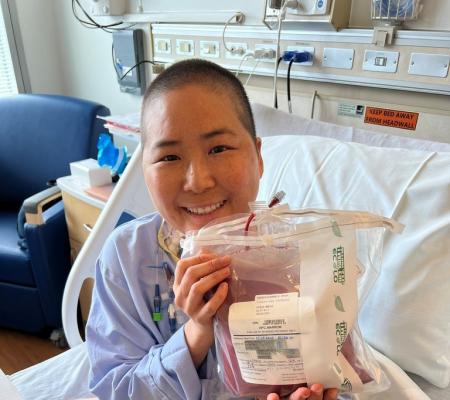
Babies with SCID lack a functioning immune system, making them vulnerable to fatal infections unless they are treated in infancy with a bone marrow transplant (BMT), also known as hematopoietic stem cell transplantation (HSCT), or clinical trial gene therapy.
The new study from PIDTC is a retrospective analysis examining how various factors affected the survival of patients diagnosed with SCID across almost four decades. The paper focuses in particular on how the institution of population-based NBS impacted survival.
In a study of 902 patients treated with BMT at 34 PIDTC centers, researchers examined data from several time periods beginning in 1982. They found that for the first three time periods, covering 28 years total, the five-year survival rate of SCID patients treated with BMT hovered at 72-73%. However, in the period from 2010–2018, corresponding to when states instituted NBS for SCID, five-year survival rose to 87%.
“What was really fascinating was that the overall survival didn’t change for the first three decades of our data collection, and then suddenly, from 2010 to 2018, there was a significant jump. So, what changed after all that time?” said Dr. Jennifer Puck, University of California San Francisco (UCSF) immunologist and PIDTC principal investigator, during a presentation at the Clinical Immunology Society (CIS) 2023 Annual Meeting.
“It wasn’t that we were doing transplants a lot differently. Yes, the matched, unrelated donor registry was growing but that couldn’t account for all of this and what we realized is that NBS had been increasingly adopted by states, starting in 2008 actually, but the first PIDTC enrollees were in 2010, and maybe that would account for this increase.”
To probe how the survival of SCID patients treated with BMT evolved, researchers examined risk factors for poor BMT outcomes, including “triggers,” or the reason a child was originally suspected of having SCID. Those triggers included a family history of SCID, clinical illness, and NBS.
During the eight-year period when states gradually added SCID to their NBS panels, babies diagnosed with SCID through NBS experienced a five-year survival rate of 92.5%, better than babies diagnosed through family history (85.4%) or clinical infection (79.9%).
However, because of the pace of implementation of NBS, some groups still had worse outcomes from 2010 to 2018. Those babies with an active infection, older age at transplant, and genotypes including DNA repair defects such as Artemis SCID and ADA-SCID, as well as Black infants, were at greater risk.
Another important finding of the study is that once states instituted NBS, BMT “no longer conveyed a survival advantage over earlier time intervals,” according to the study. Researchers determined that early diagnosis, specifically before three-and-half-months old, and not having an infection at the time of treatment were the factors improved by NBS that ultimately contributed to better overall survival.
“After initiations of SCID newborn screening, enhanced survival of patients with SCID has been observed in the USA and Canada that is independent of advances in preventing infections and transplantation procedures. Despite differences in local medical practices, the ability to identify infants with SCID early through newborn screening and to provide allogeneic HCT before the onset of life-threatening infections has the potential to save lives worldwide,” concluded the study.
Related resources
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.




The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.