-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can manage it. Learn about PI diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Research Grant Program
-
Consulting immunologist
-
Diagnosing PI
-
Getting prior authorization
-
Clinician education
-
Survey research
-
Participating in clinical trials

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Research Grant Program
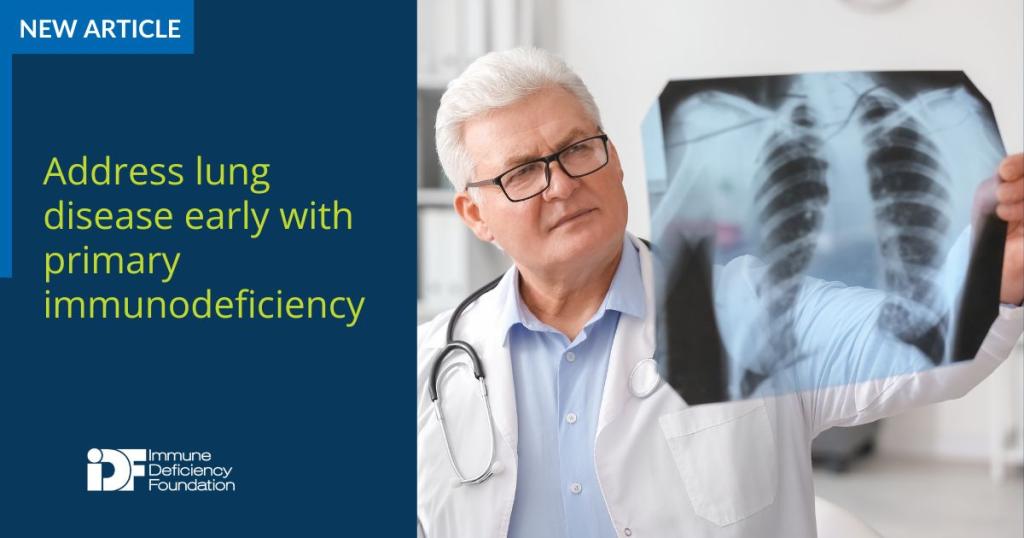
Primary immunodeficiency (PI), also known as inborn errors of immunity (IEI), increases the risk of developing lung disease, leading to other serious health conditions affecting the heart, liver, kidney, and brain in patients with PI. Recognizing early signs of lung, or pulmonary, disease in PI is essential for prompt diagnosis and treatment, improving long-term mortality and morbidity, and preventing and reducing its progression.
“Pulmonary disease is the most common cause of end-organ damage in patients with immunodeficiency,” said Dr. Antoine Azar, interim director of the Division of Allergy and Clinical Immunology and director for the Adult Primary Immunodeficiency Center at Johns Hopkins University, who spoke on PI and respiratory health at the 2024 PI Conference.
“It can often be the initial manifestation of an immunodeficiency. I have several patients referred to me from pulmonologists because this is where the patients were coming to all the time with either inflammatory disease or recurrent infections.”
A person with PI experiences pulmonary infections that differ from those of someone without a compromised immune system.
PI may cause frequent cases of pneumonia and severe infections that affect multiple parts of the lung. Pneumonia can also progress to complications such as infected fluid around the lungs or a lung abscess. Recovery can require months of antibiotics and even hospitalization.
Persons with PI are also more vulnerable to infection from organisms that don’t typically cause illness in those without PI such as Pneumocystis, Pseudomonas, Aspergillus, or cytomegalovirus (CMV).
Since recurrent cases of pneumonia could be caused by other factors, like structural abnormalities in the lungs, stomach reflux affecting the lungs, or cystic fibrosis, providers should rule out other conditions first.
“It's important with these pneumonias to be very clear as to where these pneumonias are. Are they always in the same spot? What did the X-ray show? What does a CT scan show?” said Azar, referencing two common lung imaging tests.
Treatment for respiratory infections includes antibiotics, most likely for a long duration of time, the use of prophylactic antibiotics, and Ig replacement therapy.
Increased IgG through Ig replacement therapy is associated with decreased pneumonia, said Azar, who referenced a series of studies that looked at the prevalence of pneumonia in patients receiving immunoglobulin therapy. The studies showed that with each 100 milligram/dL increase in IgG trough level, the incidence of pneumonia decreased by 27%.
“Sometimes, if your IgG level is around 600 or 700 or 800, it looks like it's normal IgG but if somebody's still having recurrent respiratory infections and recurrent pneumonias despite a good IgG level it means that they may need a higher dose of immunoglobulin therapy,” said Azar.
Sometimes when infections recur, a patient can develop bronchiectasis.
“Bronchiectasis represents permanent lung damage that is usually caused by recurrent infections. So, if you have infection after infection in certain parts of the lungs, at the end, it causes this lung damage that is irreversible,” explained Azar.
“The more infections you have, the more you are at risk of developing this lung damage or bronchiectasis.”
Pulmonary function tests in bronchiectasis show that there’s obstruction in the lungs, but the most successful way to detect bronchiectasis is with a computed tomography (CT) scan. Azar said that for patients with common variable immunodeficiency (CVID), he recommends a CT scan versus an X-ray to look for bronchiectasis.
“A chest x-ray is great to look for pneumonia, but it may not be sensitive enough to detect bronchiectasis,” said Azar.
“The best way to look for bronchiectasis is a CT scan. That’s the gold standard. There are a number of findings that are typically seen in bronchiectasis that are recognized by radiologists or by the ordering physician—dilated bronchi, it’s called the signate ring sign, and a tree-in-bud pattern.”
Like lung disease in general, bronchiectasis is more common in the PI community. One study showed that in a cohort of 900 patients with CVID, about a quarter of the patients had bronchiectasis. In another study from the UK of 801 patients with CVID, 47% of the group had bronchiectasis.
“It’s an important thing to look for and screen for,” said Azar.
A third category of pulmonary illness prevalent in the PI community is interstitial lung disease, a broad term that covers a range of conditions including:
- Benign follicular bronchiolitis—swelling of the lymph nodes that occurs in the airways and is usually a benign condition.
- Lymphocytic interstitial pneumonia—swelling of the lymph nodes that is a progression of bronchiolitis.
- Nodular lymphoid hyperplasia—pulmonary nodules.
- Granulomatous lymphocytic interstitial lung disease (GLILD)—inflammation caused by clumps of immune cells that can lead to long-term lung damage and is common in CVID.
Not only does GLILD cause inflammation and scarring in the lungs, but this multi-system inflammatory disease also leads to other health complications like liver disease, an enlarged spleen, and swollen lymph nodes. With GLILD, granulomas can occur on the skin, and in the liver, brain, and gastrointestinal tract.
GLILD typically occurs in females more than males around the age of 20 to 50 and presents with gradual shortness of breath, cough, fatigue, and night sweats.
“It can also be asymptomatic and that’s why it’s important to screen for it in patients with CVID,” said Azar. “If left untreated and it progresses, it can be really bad and cause respiratory failure.”
GLILD is diagnosed with a lung biopsy and treated with immunosuppressive drugs such as steroids along with immunoglobulin (Ig) replacement therapy.
Initial screenings for lung diseases of all types include a pulmonary function test, where a patient sits in a chamber and blows into a machine that measures their airflow. A spirometry test is another evaluation in which airflow is also measured by blowing into a tube but the person is not in a chamber.
“The full pulmonary function test, which measures not only how well your flow is but the volumes of your lungs and the diffusion capacity of your lungs, is the better test that gives you much more information than the quick spirometry,” said Azar.
“We often recommend doing this test first upon diagnosis to screen patients and on a yearly basis or if there are any signs of and symptoms of deterioration of lung function. It's an easy, non-invasive way to check for lung function.”
Patients can follow these strategies for managing lung disease:
- Stop any additional insult to the lungs such as smoking or vaping.
- Exercise regularly to strengthen the respiratory and peripheral muscles.
- Use a flutter valve to clear out mucus that accumulates in the lungs (particularly effective for bronchiectasis).
Preventing infections with vaccines is also key to keeping lungs healthy. Patients should receive the yearly influenza vaccine (inactivated), the pneumococcal vaccine, the COVID vaccine, and, for those 60 and older, the RSV vaccine. Members of the household should also receive vaccines.
Watch 2024 PI Conference sessions
Missed a session or want a refresher? 2024 PI Conference session recordings are now available!
Browse sessionsTopics
Related resources
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.





The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309