-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can live with the disease or support others in your life with PI. Learn more about PI, including the various diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Research Grant Program
-
Consulting immunologist
-
Diagnosing PI
-
Getting prior authorization
-
Clinician education
-
Survey research
-
Participating in clinical trials

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Research Grant Program
Update
Is it safe to travel?
Even before the pandemic, domestic and international travel as a person with primary immunodeficiency came with a unique set of considerations. But with COVID-19 still actively spreading in most of the world, COVID-19 risk complicates travel decisions.
The general advice on taking community COVID-19 transmission, the environment for a particular activity, and the vaccination status of others into account holds, but what else should you be thinking about? Consider the following questions:
- How are you planning to get to your destination? Some modes of transportation involve being in an indoor space for long periods of time with many strangers who may or may not be vaccinated, which is the highest risk type of setting. Note that U.S. flights and trains no longer adhere to mask mandates, but some international airlines still require passengers to wear masks.
- What is the COVID-19 transmission rate at your destination and is it trending up or down? What strains are circulating? For the U.S., these numbers are available through the CDC’s COVID Data Tracker. For international destinations, Our World in Data and Reuters have case rate and trend information. For information on strains circulating in other countries, check each country's department or ministry of health.
- Are there COVID restrictions in place? Do you need specific documentation? Make sure you know if any restrictions are in place, such as business closings or the need to present verification of your vaccination status. Restrictions or requirements for travel into and out of your destination are particularly important to keep tabs on.
- What happens if you get COVID? If the worst happens, will you have access to COVID-19 treatments and any ongoing treatments for PI? Is there a mandatory isolation or quarantine period if you test positive?
- Does your medical insurance cover COVID-19 testing and treatment and/or treatment for your PI at your destination? Do you need to purchase travel medical insurance?
- What types of COVID-19 testing and treatment are available at your destination? If you are stuck at your destination because you’re ill, is routine treatment for your PI available? Remember that other countries have not necessarily approved or authorized the same treatments/medications as the U.S.
In essence, remember to do your research, both before you book a trip and before you actually travel.
Originally Published March 12, 2022
As COVID-19 mitigation measures relax, people with primary immunodeficiency or other immunocompromising conditions must navigate this transition with little official guidance. Here, we answer some of the PI community’s most common questions. Thank you to Dr. Kathleen Sullivan for providing her expert input.
Where can I find out how high COVID-19 transmission is in my community?
One of the most important factors to help gauge your individual risk is the level of COVID-19 transmission occurring in your community (or in a community you’re traveling to, if applicable). The Centers for Disease Control and Prevention (CDC), as well as state and local public health departments, make this data available through online data dashboards (for example, the CDC’s COVID Data Tracker).
The standard measure of transmission is a 7-day moving average of COVID-19 cases per 100,000 people. This metric averages the daily number of reported cases over 7 days, then divides that average by the jurisdiction's total population. The resulting case rate can then be compared to that of other jurisdictions.
But what if the number of cases is low because not enough people are being tested? Another useful number is the percentage of positive COVID-19 tests, or percent positivity. If this percentage is above 5%, it may indicate that not enough tests are being performed to fully capture the extent of community transmission. In other words, true transmission could be higher than the case rate indicates.
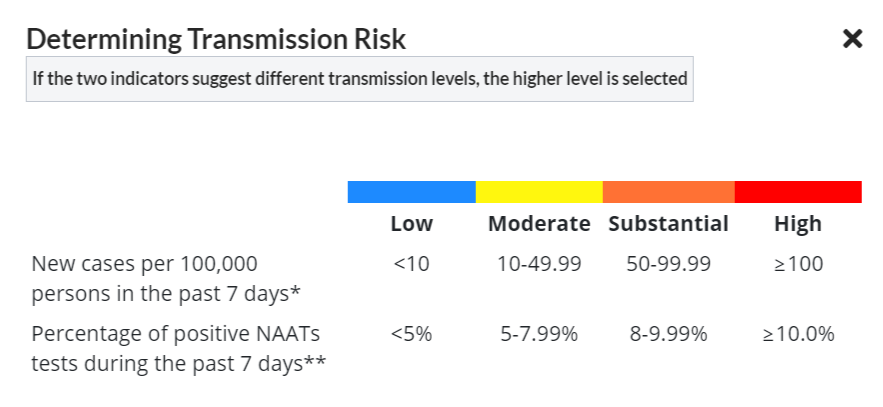
The CDC’s categorization of transmission risk using both case rate and percent positivity is useful for determining your personal risk (note that CDC transitioned to a different metric to guide COVID-19 mitigation and public health response in late February 2022). Less than 10 cases per 100,000 people is considered low transmission (provided test positivity is less than 5%), while more than 99 is considered high transmission.
Bookmark the dashboard for your area and check these numbers frequently to stay informed about the level of transmission in your community. Depending on transmission risk, you may decide to layer on extra precautions or forgo certain activities in high-risk settings.
What activities are safe for those with primary immunodeficiency?
Being around other people will always carry more risk for getting COVID-19 than isolating at home. However, isolation has mental health risks and may affect physical health as well if people delay medical care or decrease their physical activity.
There is no one definition of “safe” and we still don’t know the absolute risk of any given situation for a person with PI. However, studies show that the risk of COVID-19 transmission outdoors is much lower than indoors. Outdoor activities also allow for greater social distancing and are the safest types of activities to engage in as a person with PI.
Gathering indoors with people you know are vaccinated and boosted is riskier than being outdoors, but not as risky as gathering indoors with people of unknown vaccination status.
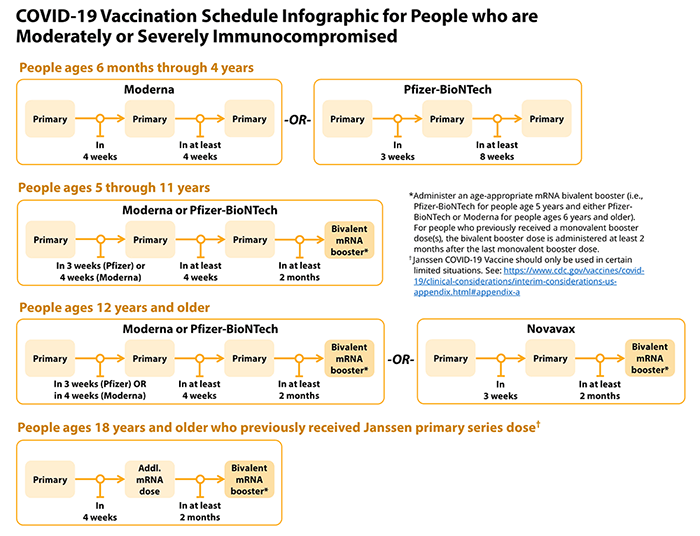
People who are not vaccinated continue to be at greater risk of becoming infected with SAR-CoV-2 and transmitting it to others compared to those who are fully vaccinated and boosted. For this reason, it is very important that household members of those with PI stay up to date on vaccinations and booster shots.
Being indoors in public when you are not in contact with any particular person for long, such as grocery shopping, is likely on par with prolonged indoor contact (more than 15 minutes at less than 6 feet) with people you know are vaccinated and boosted. The riskiest settings involve prolonged indoor contact with people outside of your immediate household of unknown vaccine status - think indoor event venues, restaurants, bars, movie theaters, and gyms.
In any setting - outdoors, indoors with people you know are vaccinated and boosted, or indoors in public - the risk of transmission increases if you are not masked or able to social distance (stay at least 6 feet away from others).
Should those with primary immunodeficiency continue social distancing and wearing masks?
Social distancing and wearing masks are two relatively easy ways of lowering your risk of infection. Given that many jurisdictions are dropping mask mandates for the general public, you should assume that most other people will not be wearing masks in your community.
In indoor settings when your community has low transmission, masking is not necessary and can be a personal decision based on your comfort level. At moderate transmission, you should wear the most protective type of mask that you can reasonably obtain (i.e., is readily available and not too expensive). If your community has substantial or high transmission, use an N95 or equivalent mask, like KN95 or KF94, in indoor settings and avoid places where social distancing is not possible. Note that N95, KN95, and KF94 masks can be reused until they get wet or have obvious dirt on them.
While N99 masks do offer more protection than N95, they are difficult to obtain and expensive. They filter out 99% of 300 nm particles (compared to 95% for N95s), but the SARS-CoV-2 virus is much smaller than that. So, N99 masks are not ‘virus proof.’
Closing Thoughts
Do what you can to reasonably minimize your COVID-19 risk. Make sure you are fully vaccinated and boosted even if you have an antibody deficiency. Most people with PI mount a protective antibody response to the COVID-19 vaccine. For those who don’t (people with X-linked agammaglobulinemia (XLA) and some patients with common variable immunodeficiency (CVID)), vaccination may still provide you with T cell protection against severe disease. If transmission is moderate, substantial, or high in your community, wear a mask indoors and practice social distancing in public.
Also, keep in mind that we now have more treatment options for those who do become infected and that the Omicron variant tends to cause less severe disease. Overall, those with PI should be able to venture out into the world again. But make sure you keep an eye on community transmission!
This content should not be used as a substitute for professional medical advice. In all cases, patients and caregivers should consult their healthcare providers. Each patient’s condition and treatment is unique.
Related resources
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.





The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309