-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can live with the disease or support others in your life with PI. Learn more about PI, including the various diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Research Grant Program
-
Consulting immunologist
-
Diagnosing PI
-
Getting prior authorization
-
Clinician education
-
Survey research
-
Participating in clinical trials

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Research Grant Program
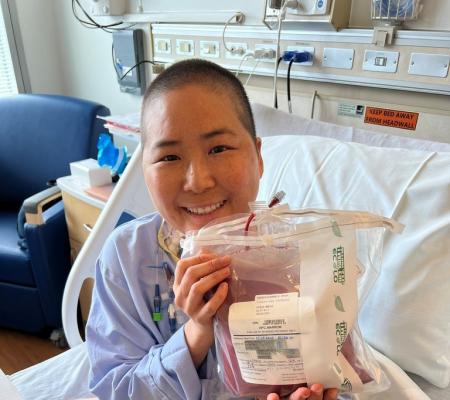
SCID Compass recently convened a panel of experts to discuss chimerism—an often daunting and confusing term—and how it plays a role in the recovery of babies with severe combined immunodeficiency (SCID) who receive bone marrow transplants (BMT).
“What is chimerism?,” moderated by Dr. Ami Shah from the Stanford University School of Medicine, featured Dr. Mort Cowan from the University of California San Francisco, Dr. Robertson Parkman from Children’s Hospital Los Angeles, and Dr. Ken Weinberg from the Stanford University School of Medicine. All three are members of CalSCID, a California-based program designed to examine and address the long-term follow-up care needs of families with SCID and T-cell lymphoma.
“As a group, we need to do a better job at explaining what chimerism is,” said Weinberg.
The term ‘chimera’ refers to any organism with cells that do not all have the same DNA, in reference to the creature from Greek mythology that had a lion’s head, a goat’s body, and a serpent’s tail. When a baby with severe combined immunodeficiency (SCID)—or a different type of primary immunity such as Wiskott-Aldrich syndrome (WAS), for example—receives a bone marrow transplant (BMT), they become recipients of a donor’s blood-forming stem cells. These stem cells in the bone marrow, and the blood and immune system cells they make contain the donor’s DNA. After a successful BMT, the recipient has a mixture of their own cells and the donor cells, making them a chimera.
In the case of SCID, the goal is for the healthy immune cells that the donor’s stem cells make to provide the recipient with a functioning immune system. One of the ways doctors determine whether the bone marrow transplant is working is by examining the chimerism, or percentage of donor versus recipient immune system cells, in a patient. The higher the percentage of donor chimerism in a patient, the more donor cells the patient has, and the better the outcome for the patient, in general.
While a bone marrow transplant may seem straightforward, a host of variables affect the success of the procedure.
First, donor cells vary in their stage of development—some are newer (or baby) stem cells, some are committed progenitor (or teenage) cells, and others are mature (or adult) cells—and replenish the baby’s immune system in different ways.
Mature, or adult, cells can be both helpful and harmful.
“The graft will have various levels of mature T cells, and the great advantage is that they can fight an infection soon after transplant,” said Weinberg.
On the other hand, mature T cells in a graft can cause complications, such as graft versus host disease (GVHD), a condition in which the donor cells attack the recipient leading to organ damage and other life-threatening health problems. Therefore, sometimes doctors provide what is called a T-cell-depleted transplant to prevent GVHD.
Mature T cells also may have a short lifespan and die off quickly, rendering them less effective.
The committed progenitor, or teenage, cells don’t cause GVHD, but they do take many months to mature, and there’s no guarantee they will grow into T cells. They are restricted in their development and only become certain kinds of cells.
The newer, or baby, stem cells can become any kind of cell, including T cells.
“One of the signs that someone has a graft of stem cells is that the various blood cells—not just their T cells—are coming from the donor, and we have developed molecular ways to tell the difference between donor cells that came from the donor and cells that are your own,” said Weinberg.
If all of the child’s blood cells after the transplant come from their donor, then they are a full chimera or have full donor chimerism. If some of their blood cells come from their donor and others are their own, then they are a mixed chimera or have mixed chimerism.
Whether someone has full or mixed chimerism depends on the following factors:
- What kind of SCID do they have? While all SCID results in a lack of properly functioning T cells, some types of SCID allow a baby to produce non-functional B cells or natural killer (NK) cells (two other important immune system cells in addition to the T cell). Depending on their type of SCID, a baby with a transplant might produce B cells that are their own or B cells from the donor, for example.
- What medications did the baby have as conditioning before the transplant? Conditioning makes room in the bone marrow for the transplant. Conditioning can be heavy-dose or reduced-intensity chemotherapy but also other drugs. Different drugs have different effects on chimerism. Receiving no conditioning also affects chimerism.
- What type of graft (transplant) did the child receive? They may have had a T-cell-depleted graft where the T cells were removed or an unmanipulated graft in which all the cells were given.
- What infections did the baby have prior to the transplant?
To further explain the complexity of chimerism, the doctors examined three cases of children with SCID who received transplants and their outcomes.
The doctors first discussed a baby boy with X-linked SCID who received a BMT without conditioning from his tissue-matched sister at four months old. He had no T cells and non-functioning B and NK cells before the transplant.
At seven months, all his T cells were from the donor (full T cell chimerism), but he had only minimal chimerism with B cells (4% chimerism) and NK cells (7% chimerism). Because doctors didn’t give conditioning, that accounts for the low chimerism with the B and NK cells.
“Since we didn’t give any conditioning, or we didn’t make space, we didn’t give any chemotherapy to make space in the bone marrow, then you would not expect very many, if any, stem cells from the donor to actually engraft,” said Cowan.
Would the lack of functioning B cells (which produce antibodies) mean the child needs immunoglobulin replacement therapy to replenish antibodies?
Yes, said Cowan, but you need more time than 100 days (Day 100 is an important threshold when measuring BMT success) to fully determine if the B cells will function. In over 70% of cases of X-linked SCID transplanted with a matched sibling, even without conditioning, the children do develop some B cell immunity eventually, said Cowan.
“That’s something that will have to be evaluated over time. So, that's one reason why we don't just say goodbye to the patient after a hundred days and send them on their way. Even if they have good T cells, we do have to follow them and check to see whether they're able to make immunoglobulins. And if they are, whether they can make specific antibody responses,” said Cowan.
“With such a low donor chimerism, I'd be a little concerned or pessimistic about whether B cell immunity is going to recover. But it takes time. It can take a year or two before you really know whether B cell immunity is going to be restored.”
That’s why long-term follow-up for SCID is so critical, said Shah.
“It’s really important for these patients to continually monitor that chimerism so we know if the stem cells continue to grow or do we just have a mature T cell graft. And we also need to monitor their immunity long-term because patients aren't just transplanted and then go away. We want to make sure we continue to follow these patients to make sure that we're doing the best to prevent them from getting infections,” said Shah.
In the second case, doctors treated a baby with Omenn’s syndrome with conditioning drugs to eliminate his existing overreactive T cells that caused GVHD and make space for a T-cell-depleted transplant from his father. The transplant resulted in mixed chimerism at Day 100 – 60% of all cells were the baby’s own, and 40% were his father’s. Sorted chimerism showed that 90% of T cells were the baby’s own, and 100% of B cells and NK cells came from the father.
To improve the baby’s prognosis, doctors provided suggestions, including a second transplant with drugs to eliminate the T cells or administering T cell-depleting drugs with no second transplant to eliminate the T cells.
Cowan said each patient’s case is unique and dictates how to move forward with treatment.
“The most important thing is that if this situation does happen for you as a patient or as a family, have a long conversation with your physician and go through all the different options that are available and really understand what those cells that you currently have are and what that means long-term,” said Shah.
The third case discussed by doctors proved even more difficult. A baby with SCID engrafted with the mother’s T cells in utero and was suffering an RSV infection and pneumonia requiring a ventilator at the time of transplant. The child received reduced-intensity conditioning and a T-cell-depleted transplant from his mother. On Day 100, he had 100% donor chimerism with T cells, 80% donor chimerism with B cells, and 90% donor chimerism with NK cells. However, at a year old, the boy’s T cells had dropped very low.
Doctors said the T cell environment—the thymus—may have been damaged early in life by GVHD because of the maternal T cells circulating in his body, and the question was, will the boy begin to make T cells at some point? Options include treating with Ig therapy and waiting longer for T cell development, providing the baby with a second transplant, or even possibly performing a thymic transplant on the baby.
“One of the things that this case really illustrates is that when patients do well, they do really well. When patients have mixed chimerism at good levels with the majority of them still being from the donor, we probably are okay. We may need to give a few more medications, but we're probably okay. But when we have a very low number of immune reconstitution, and we have low chimerism, that's when we really have to jump in and think about what to do, what's best for the patient,” said Shah.
Several factors about a patient contribute to how doctors decide to proceed with difficult cases post-transplant:
- Did they receive conditioning, and if so, what kind?
- Do they have infections?
- Do they have any GVHD?
“That’s why the answer sometimes in patients that are very complicated like this is not so easy. As a group of people that take care of SCID patients, we oftentimes work with our colleagues across the country together to think through what are some of the best options available,” said Shah. “There's not a one-size-fits-all for patients when they have this degree of low chimerism.”
The importance of having long-term follow-up appointments either at the transplant institution or locally is essential so that doctors can monitor a patient’s immune system and the level of chimerism.
“Some of you may have had a transplant many years ago and are now adults. So, you weren't privy to all this information when you were a baby. But it's really important as you become an adult that you think through, what is going on with me now? What did I have? And where am I now? And what does that mean for me long-term?” said Shah.
Chimerism can be very complicated, and if patients don't understand what their chimerisms mean, they should ask their doctor to explain, said Shah.
“Our best way of taking care of you as patients is making sure you understand the importance of what your test results mean so that you can make informed decisions and you know what your restrictions may be and what you can and cannot do,” she said.
Screen documentary
Host a private screening of Compromised: Life Without Immunity to experience the resilience, hope, and determination of the PI community. And know that your hosted event can be two people or 100+!
Watch the filmThis page contains general medical and/or legal information that cannot be applied safely to any individual case. Medical and/or legal knowledge and practice can change rapidly. Therefore, this page should not be used as a substitute for professional medical and/or legal advice. Additionally, links to other resources and websites are shared for informational purposes only and should not be considered an endorsement by the Immune Deficiency Foundation.
Related resources
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.





The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309