
-
Understanding primary immunodeficiency (PI)

Understanding PI
The more you understand about primary immunodeficiency (PI), the better you can live with the disease or support others in your life with PI. Learn more about PI, including the various diagnoses and treatment options.
-
Living with PI
-
Addressing mental health
-
Explaining your diagnosis
- General care
- Get support
- For parents and guardians
-
Managing workplace issues
- Navigating insurance
-
Traveling safely

Living with PI
Living with primary immunodeficiency (PI) can be challenging, but you’re not alone—many people with PI lead full and active lives. With the right support and resources, you can, too.
-
Addressing mental health
-
Get involved

Get involved
Be a hero for those with PI. Change lives by promoting primary immunodeficiency (PI) awareness and taking action in your community through advocacy, donating, volunteering, or fundraising.
-
Advancing research and clinical care
-
Research Grant Program
-
Consulting immunologist
-
Diagnosing PI
-
Getting prior authorization
-
Clinician education
-
Survey research
-
Participating in clinical trials

Advancing research and clinical care
Whether you’re a clinician, researcher, or an individual with primary immunodeficiency (PI), IDF has resources to help you advance the field. Get details on surveys, grants, and clinical trials.
-
Research Grant Program
Update - As predicted, the 2022-2023 respiratory virus season has started early and hit hard. In addition to high rates of seasonal influenza, the U.S. Centers for Disease Control and Prevention (CDC) is warning about high levels of respiratory syncytial virus (RSV).
RSV is a very common virus that most children encounter before two years of age. Symptoms are similar to the flu, including coughing, sneezing, runny nose, and a fever. RSV spreads through respiratory droplets produced by coughing and sneezing and can survive on hard surfaces (fomites) for hours.
In some cases, RSV can cause severe disease, including inflammation of the air sacs (pneumonia) and/or small airways (bronchiolitis) in the lungs, that requires hospitalization for breathing support or dehydration. Those who are experiencing trouble breathing or signs of dehydration should seek immediate medical attention.
Children under six months old or born prematurely, anyone with a compromised immune system or chronic lung or heart disease, and adults over 65 are at higher risk for developing severe RSV. Studies have shown that RSV can be particularly dangerous in those with types of primary immunodeficiency that impair cellular immune responses (for example, those with combined immunodeficiencies).
Unfortunately, there currently are no vaccines for RSV, although several are in development. There is a monoclonal antibody called palivizumab (trade name Synagis) that is approved by the U.S. Food and Drug Administration (FDA) for the prevention of RSV in certain young children. It is typically given as an injection once a month for up to five consecutive months. The American Academy of Pediatrics (AAP) recently recommended its use in eligible children for more than five consecutive months if RSV activity remains high.
For those who are not eligible for palivizumab, the CDC recommends general respiratory virus prevention measures, including washing hands, limiting contact with sick individuals, and disinfecting surfaces. Masking may also prevent the spread of RSV, as it does for COVID-19.
Originally published October 14, 2022
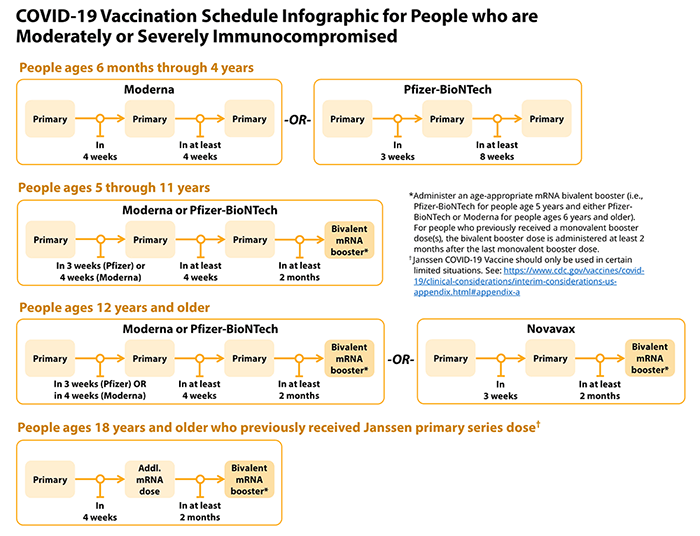
On October 12, 2022, the U.S. Food and Drug Administration authorized, and the Centers for Disease Control and Prevention (CDC) recommended, bivalent COVID-19 boosters for children ages five and up. Previously, these boosters, which provide protection against the original strain of SARS-CoV-2 and the BA.4 and BA.5 Omicron subvariants, were authorized only for those 12 and older. As with older individuals, CDC recommends that those five through 11 years of age receive a bivalent booster two months after a prior COVID-19 vaccine dose (either primary series or booster) or three months after a COVID-19 infection.
https://www.cdc.gov/vaccines/covid-19/clinical-considerations/interim-considerations-us.html#immunocompromised
Originally published September 7, 2022
As we head into cold and flu season still battling COVID-19, it’s important to know how to keep healthy and what to do if you get sick.
Colds, the flu, and COVID-19 are all caused by viruses and spread from person to person through respiratory droplets and contaminated surfaces (also known as fomites). Flu season in the U.S. is generally from December to February, but can start earlier or linger later. Although the U.S. Centers for Disease Control and Prevention (CDC) doesn’t track the common cold, you can keep up with weekly flu and COVID-19 activity in your area through trackers on the CDC website.
What Experts Are Forecasting
Early in the pandemic, public health officials worried about a ‘twindemic’ of COVID-19 and the flu. In fact, seasonal flu rates have been low for the past two seasons (2020-2021 and 2021-2022), largely due to COVID-19 mitigation measures like masking, social distancing, and lockdowns.
However, masking and social distancing have been widely abandoned. Recent mild flu seasons have also dropped population immunity, particularly among young children, as have lower flu vaccination rates. For these reasons, experts expect cold and flu viruses to make a roaring comeback this year.
If Australia is any indication, experts are right. From mid-April to July, the number of confirmed flu cases in Australia exceeded the numbers for every year since 2017.
Vaccinate, Vaccinate, Vaccinate
The most important step you can take to stay healthy is to make sure you get vaccinated against the flu and are up to date on COVID-19 vaccinations and boosters. All household and other close contacts of individuals with PI should also prioritize getting vaccinated.
Note that the live flu vaccine, which is administered as a nasal spray, is not recommended for those who are immunocompromised. Also note that immunoglobulin (Ig) products may not have protective levels of antibodies against current flu strains because manufacturing takes six months or more from the initial plasma donation. So, even if you don’t typically get vaccines, most people with PI should receive the inactivated seasonal flu vaccine—talk to your healthcare provider about what’s right for you.
This year’s inactivated flu vaccine is quadrivalent, which means it protects against four different influenza strains. The CDC recommends getting your flu shot in September or October so that immunity lasts through the entire season.
It’s also important to stay up to date on COVID-19 primary series vaccines and booster shots. Individuals with moderately to severely immunocompromising PI should receive at least three doses of COVID-19 vaccine, depending on age and type of vaccine.
COVID-19 bivalent booster shots that protect against the original Wuhan strain as well as the BA.4 and BA.5 Omicron subvariants are available and recommended for most people 12 and older. The CDC recommends that people who are immunocompromised receive the bivalent booster two months after their last vaccine dose, regardless of whether that dose was part of a primary series or a previous booster. Use the CDC’s COVID-19 booster tool to find out if you are due for a booster.
Other Ways to Stay Healthy
The good news is that basic hygiene practices, like properly washing your hands, boosting indoor ventilation, disinfecting high-touch surfaces, and distancing from people showing signs of illness, can help you avoid colds, the flu, and COVID-19.
Individuals with PI may also want to continue social distancing and wearing masks indoors. These measures reduce transmission of respiratory viruses in general, so they are effective for avoiding all three illnesses. Although any mask is better than no mask, masks that are certified as N95, KN95, or KF94 and fit the wearer so that air does not leak through the edges offer the best protection.
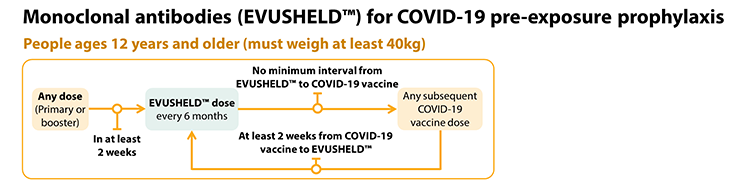
You may also want to talk to your healthcare provider about your eligibility for Evusheld, a monoclonal antibody authorized for the prevention of COVID-19 in those who are immunocompromised. Note that some healthcare providers are still not aware of this protective treatment or are misinformed about eligibility and access, so you may need to bring your healthcare provider this information. There is also a hotline that providers can call for information: 1-833-EVUSHLD.
The CDC recommends repeat dosing with Evusheld at six-month intervals to maintain protection. If you are combining Evusheld with COVID-19 vaccine doses, make sure you receive Evusheld at least two weeks after your latest vaccine dose. However, you can receive a vaccine dose without any waiting period after you receive Evusheld.
https://www.cdc.gov/vaccines/covid-19/clinical-considerations/interim-considerations-us.html#immunocompromised
Which Illness Is It?
If you start to feel sick, determining which illness you have is important so that you can get the right treatment quickly. In terms of symptoms, colds tend to be milder than the flu or COVID-19. For example, body aches or headache are common with flu or COVID-19, but not with a cold. Fever and chills are also more common with the flu or COVID-19, though many people with PI do not respond to infection with a fever.
Be prepared by having a testing plan:
- Keep unexpired rapid antigen tests for COVID-19 on hand (note that the FDA has extended the shelf life of several tests, so check their list before you throw out 'expired' tests). Remember that these tests work best if you test at least twice, several days apart. See manufacturers’ instructions for specific timing.
- There are no equivalent home tests available for the flu, but many pharmacies and doctor’s offices offer rapid flu tests. Check to see where you can get a rapid flu test and if you need a prescription to do so.
- Labcorp also offers a mail-in, non-prescription molecular test that distinguishes between the flu, COVID-19, and respiratory syncitial virus (RSV) and has been authorized by the U.S. Food and Drug Administration (FDA).
You should also have a treatment plan worked out with your healthcare provider because antiviral medications for the flu and antiviral and monoclonal antibody treatments for COVID-19 work best during the first few days of symptoms. Know which treatment(s) your healthcare provider recommends for you and why, plus where you can get it.
Related resources
Sign up for updates from IDF
Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time.





The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency.
We foster a community that is connected, engaged, and empowered through advocacy, education, and research.
Combined Charity Campaign | CFC# 66309




